Supraventricular Tachycardia
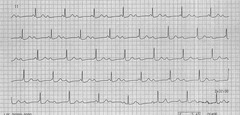
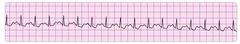
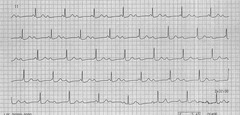
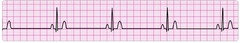
Second deg AV block: Mobitz 1
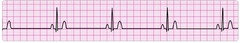
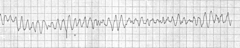
Second deg AV block: Mobitz 2
Intermittent non-conducted P waves without progressive prolongation of the PR interval (compare this to Mobitz I).
Pulseless electrical activity
Push Epi Always
Second deg AV block: Mobitz 2
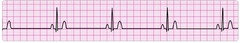
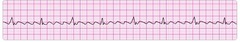
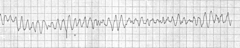
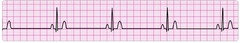
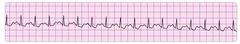
Supraventricular tachycardia
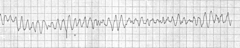
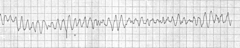
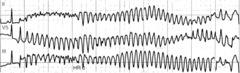
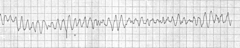
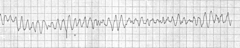
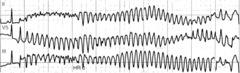
Polymorphic ventricular tachycardia
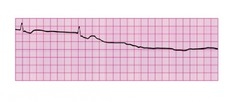
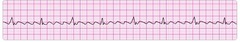
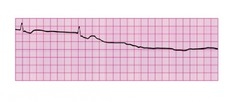
Agonal rhythm into asystole
If patient is in cardiac arrest and the rhythm is asystole and CPR is beign given. What is the first drug you should give?
(a) Atropine 0.5 mg IV/IO
(b) Atropine 1 mg IV/IO
(c) Dopamine 2 to 20 mcg/kg per min IV/IO
(d) Epinephrine 1 mg IV/IO
(d) Epinephrine 1 mg IV/IO
A patient has a rapid irregular wide-complex tachycardia. The ventricular rate is 138 bpm. He is asymptomatic, with a blood pressure of 110/70. He has a history of angina. What action is recommended next?
(a) Giving adenosine 6 mg IV bolus
(b) Giving lidocaine 1 to 1.5 mg IV bolus
(c) Performing synchroniczed cardioversion
(d) Seeking expert consultation
(d) Seeking expert consultation
A patient is in cardiac arrest. Ventricular fibrillation has been refractory to a second shock. Which drug should be administered first?
(a) Atropine 1 mg IV/IO
(b) Epinephrine 1 mg IV/IO
(c) Lidocaine 1 mg/kg IV/IO
(d) Sodium bicarbonate 50 mEq IV/IO
(b) Epinephrine 1 mg IV/IO
You arrive on the scene with the code team. High-quality CPR is in progress. An AED has previously advised "no shock indicated." A rhythm check now finds asystole. After resuming high-quality compressions, which action do you take next?
(a) Call for a pulse check
(b) Establish IV or IO access
(c) Insert a laryngeal airway
(d) Perform endotracheal intubation
(b) Establish IV or IO access
A patient is in pulseless ventricular tachycardia. Two shocks and 1 dose of epinephrine have been given. Which drug should be given next?
(a) Adenosine 6 mg
(b) Amiodarone 300 mg
(c) Epinephrine 3 mg
(d) Lidocaine 0.5 mg/kg
(b) Amiodarone 300 mg
A 35 yr old female has palpitation, light-headedness, and a stable tachycardia. The monitor shows a regular narrow-complex QRS at a rate of 180/min. Vagal manuevers have not been effective in terminating the rhythm. An IV has been established. Which drug should be administered?
(a) Adenosine 6 mg
(b) Atropine 0.5 mg
(c) Epinephrine 2 to 10 mcg/kg per minute
(d) Lidocaine
(a) Adenosine 6 mg
Pt is in refractory ventricular fibrilation. CPR is in progress. 1 dose of epinephrine given after second shock. An antiarrhythmic drug was given immediately after third shock. Which med is next?
(a) Epinephrine 1 mg
(b) Epinephrine 3 mg
(c) Sodium bicarb 50 mEq
(d) Second dose of antiarrhythmic drug
(a) Epinephrine 1 mg
What is the indication for use of magnesium in cardiac arrest?
(a) Ventricular tachycardia associated with a normal QT interval
(b) Shock-refractory monomorphic ventricular tachycardia
(c) Pulseless ventricular tachycardia-associated torsades de pointes
(d) Shock-refractory ventricular fibrillation
(c) Pulseless ventricular tachycardia-associated torsades de pointes
A pt is in cardiac arrest. Ventricular fibrillation has been refractory to an initial shock. If no pathway for medication administration is in place, which method is preferred?
(a) Central line
(b) Endotracheal tube
(c) External jugular vein
(d) IV or IO
(d) IV or IO
Which intervention is most appropriate for the treatment of a patient in asystole?
(a) Atropine
(b) Defibrillation
(c) Epinephrine
(d) Transcutaneous pacing
(c) Epinephrine
You are caring for a 66 yr old man with a hx of a large intracerebral hemorrhage 2 months ago. He is being evaluated for another acute stroke. The CT scane is negative for hemorrhage. The pt is receiving oxygen via nasal cannula at 2 L/min, and an IV has been established. His BP is 180/100. Which drug do you anticipate giving to this pt?
(a) Aspirin
(b) Glucose (D50)
(c) Nicardipine
(d) rTPA
(a) Aspirin
Pt is in refractory ventricular fibrillation and has received multiple appropriate defibrillation shocks, epinephrine 1 mg IV twice, and an initial dose of amiodarone 300 mg IV. Pt is intubated. Which best describes the recommended second dose of amiodarone for this pt?
(a) 1 mg/kg IV push
(b) 1 to 2 mg/min infusion
(c) 150 mg IV push
(d) 300 mg IV push
(c) 150 mg IV push
A monitored pt in the ICU developed a sudden onset of narrow-complex tachycardia at a rate of 200. Pt's BP is 128/58, PETCO2 is 38, and pulse oximetry reading is 98%. There is vascular access in the left arm, and pt has not been given any vasoactive drugs. 12 lead EKG confirms a supraventricular tachycardia w/ no evidence of ischemia or infarction. Heart rate has not responded to vagal manuevers. What is your next action?
(a) Administer adenosine 6 mg IV push
(b) Administer amiodarone 300 mg IV push
(c) Perform synchronized cardioversion at 50 J
(d) Perform synchronized cardioversion at 200 J
(a) Administer adenosine 6 mg IV push
In which situation does bradycardia require treatment?
(a) 12-lead ECG showing a normal sinus rhythm
(b) Hypotension
(c) Diastolic blood pressure > 90
(d) Systolic blood pressure > 100
(b) Hypotension
A 67 yr old woman has palpitations, chest discomfort, and tachycardia. The monitor shows a regular wide-complex QRS at a rate of 180/min. She becomes diaphoretic, and her blood pressure is 80/60. Which action do you take next?
(a) Establish IV access
(b) Obtain a 12 lead EKG
(c) Perform electrical cardioversion
(d) Seek expert consultation
(c) Perform electrical cardioversion
Pt w/ sinus bradycardia and a heart rate of 42 has diaphoresis and a blood pressure of 80/60. What is the initial dose of atropine?
(a) 0.1 mg
(b) 0.5 mg
(c) 1 mg
(d) 3 mg
(b) 0.5 mg
A pt w/ STEMI has ongoing chest discomfort. Heparin 4000 units IV bolus and a heparin infusion of 1000 units per hr are being administered. The pt did not take aspirin because he has a hx of gastritis, which was treated 5 yrs ago. What is your next action?
(a) Give aspirin 160 to 325 mg to chew
(b) Give clopidogrel 300 mg orally
(c) Give enteric-coated aspirin 75 mg orally
(d) Give enteric-coated aspirin 325 mg rectally
(a) Give aspirin 160 to 325 mg to chew
62 yr old man suddenly expereinced difficulty speaking and left-sided weakness. He meets initial criteria for fibrinolytic therapy, and a CT scan of the brain is ordered. Which best describes the guidelines for antiplatelet and fibrinolytic therapy?
(a) Give aspirin 160 to 325 mg to be chewed immediately
(b) Give aspirin 160 mg and clopidogrel 75 mg orally
(c) Give heparin if the CT scan is negative for hemorrhage
(d) Hold aspirin for at least 24 hrs if rtPA is administered
(d) Hold aspirin for at least 24 hrs if rtPA is administered
A patient has sinus bradycardia w/ a heart rate of 36. Atropine has been administered to a total dose of 3 mg. A transcutaneous pacemaker has failed to capture. The pt is confused, and her BP is 88/56. Which therapy is now indicated?
(a) Atropine 1 mg
(b) Epinephrine 2 to 10 mcg/min
(c) Adenosine 6 mg
(d) Normal saline 250 mL to 500 mL bolus
(b) Epinephrine 2 to 10 mcg/min
A 45 yr old woman with a hx of palpitations develops light-headedness and palpitations. She has received adenosine 6 mg IV for the rhythm shown here, without conversion of the rhythm. She is now extremely apprehensive. Her BP is 128/70 mm Hg. What is the next appropriate intervention?
(a) Administer adenosine 12 mg IV
(b) Perform unsynchronized cardioversion
(c) Perform vagal maneuvers
(d) Perform synchronized cardioversion
(a) Administer adenosine 12 mg IV
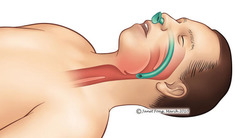
Which action is likely to cause air to enter the victim's stomach (gastric inflation) during bag-mask ventilation?
(a) Giving breaths over 1 second
(b) Ventilating too quickly
(c) Providing a good seal btwn the face and mask
(d) Providing just enough volume for chest to rise
(b) Ventilating too quickly
What is the recommended depth of chest compressions for an adult victim?
At least 2 inches
You are the code team leader and arrive to find a patient with CPR in progress. On the next rhythm check, you see electrical activity on the monitor. She has no pulse or respirations. Bag-mask ventilations are producing visible chest rise, and IO access has been established. Which intervention would be your next action?
(a) Atropine 1 mg
(b) Dopamine at 10 to 20 mcg/kg per min
(c) Epinephrine 1 mg
(d) Intubation and administration of 100% oxygen
(c) Epinephrine 1 mg
How often should you switch chest compressors to avoid fatigue?
Every 2 minutes
You are providing bag-mask ventilation to a pt in respiratory arrest. How often should you provide ventilations?
About every 5-6 secs
Which intervention is most important in reducing this patient's in-hospital and 30 day mortality rate?
(a) Application of transcutaenous pacemaker
(b) Atropine administration
(c) Nitroglycerin administration
(d) Reperfusion therapy
(d) Reperfusion therapy
How does complete chest recoil contribute to effective CPR?
(a) Allows maximum blood return to the heart
(b) Reduces rescuer fatigue
(c) Reduces the risk of rib fractures
(d) Increases the rate of chest compressions
(a) Allows maximum blood return to the heart
A patient was in refractory ventricular fibrillation. A third shock has just been administered. Your team looks to you for instructions. What is your next action?
(a) Check the carotid pulse
(b) Give amiodarone 300 mg IV
(c) Give atropine 1 mg IV
(d) Resume high-quality chest compressions
(d) Resume high-quality chest compressions
A patient has been rususcitated from cardiac arrest. During post-ROSC treatment, pt becomes unresponsive, with ventricular fibrillation. Which action is indicated next?
(a) Give an immediate unsynchronized high-energy shock (defibrillation dose)
(b) Give lidocaine 1 to 1.6 mg/kg IV
(c) Perform synchronized cardioversion
(d) Repeat amiodarone 300 mg IV
(a) Give an immediate unsynchronized high-energy shock (defibrillation dose)
What is the recommended compression rate for high-quality CPR?
100-120 compressions per min
What action minimizes the risk of air entering the victim's stomach during bag-mask ventilation?
(a) Ventilating until you see the chest rise
(b) Ventilating as quickly as you can
(c) Squeezing the bag with both hands
(d) Delivering the largest breath you can
(a) Ventilating until you see the chest rise
Which action should you take immediately after providing an AED shock?
(a) Check pulse rate
(b) prepare to deliver a second shock
(c) Resume chest compressions
(d) Start rescue breathing
(c) Resume chest compressions
After initiation of CPR and 1 shock for ventricular fibrillation, pt is still in ventricular fibrillation at next rhythm check. A second shock is given, and chest compressions are resumed immediately. An IV is in place, and no drugs have been given. BBag-mask ventilations are producing visible chest rise. What is your next intervention?
(a) Administer 3 sequential (stacked) shocks at 360 J (monophasic defibrillator)
(b) Give amiodarone 300 mg IV/IO
(c) Give epinephrine 1 mg IV/IO
(d) Intubate and administer 100% oxygen
(c) Give epinephrine 1 mg IV/IO
What is the maximum interval for pausing chest compressions?
10 seconds
A 35 yr old woman presents w/ a chief complaint of palpitations. She has no chest discomfort, shortness of breath, or light-headedness. Her BP is 120/78. On EKG, it shows she is in SVT. Which intervention is indicated first?
(a) Adenosine 3 mg IV bolus
(b) Adenosine 12 mg IV slow push (over 1 to 2 min)
(c) Metoprolol 5 mg IV and repeat if necessary
(d) Vagal manuevers
(d) Vagal manuevers
Your patient is not responsive and is not breathing. You can palpate a carotid pulse. Which action do you take next?
(a) Apply an AED
(b) Obtain a 12 lead EKG
(c) Start an IV
(d) Start rescue breathing
(d) Start rescue breathing
What is more important to start for a nonresponsive patient with no pulse, putting on an AED or starting rescue breathing?
Starting rescue breathing
You arrive on scene to find CPR in progress. Nursing staff report the pt was recovering from a pulmonary embolism and suddenly collapsed. Two shocks have been delivered, and an IV has been initiated. What do you administer now?
(a) Atropine 0.5 mg IV
(b) Epinephrine 1 mg IV
(c) Endotracheal intubation
(d) Transcutaneous pacing
(b) Epinephrine 1 mg IV
A patient becomes unresponsive. You are uncertain if a faint pulse is present. An IV is in place. Which action do you take next?
(a) Begin transcutaneous pacing
(b) Start high-quality CPR
(c) Administer atropine 1 mg
(d) Administer epinephrine 1 mg IV
(b) Start high-quality CPR
If cases where ______ is the likely cause of cardiac arrest, VENTILATION becomes much more important
hypoxia
___________ correlates w/ ROSC
High quality CPR
What are the consequences of interrupting CPR?
coronary perfusion falls
__________ can help indicate coronary perfusion pressure
Capnography
Adequate CPR compression are at least
2 inches
Why should chest compressions recoil?
To ensure adequate coronary perfusion pressure
Chest compression fraction should be around
60-80%
Don't spend more than ____ seconds without compressions
10 seconds
What should the tidal volume be for adequate ventilations?
500-600 mL or half of a bag squeeze
What should be the first thing you do when you arrive on scene?
See if patient is conscious or unconscious
What do you do next If the patient is unconscious when you first arrive on scene?
Initiate BLS
If a patient is not responsive when you first arrive on scene, what should you do next?
Call code
Get AED
During BLS, should you check breathing and pulse
(a) Separately
(b) Simultaenously
(b) Simultaenously
If pt is not breathing normally but has pulse, what should you do?
Bypass chest compressions and ventilate every 5-6 seconds
After intubating someone, what should you do next?
Provide 1 ventilation every 6 seconds
What should you assess for in the Disability function of ABCDE?
Neurologic function
- Alert
- Pain
- Voice
- Unresponsive
What are the H's of PEA?
Hypovolemia
Hypoxia
H+ (acidosis)
HyperK+
HypoK+
Hypothermia
What are the T's of PEA?
Trauma
Tension PTX
Tamponade
Toxins
Thrombosis (Pulmonary or Coronary)
Why should you not excessively ventilate?
Causes gastric insufflation
Incr intrathoracic pressure
Decr venous return and CO
Decr survival
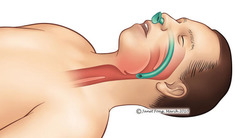
When do you use oropharyngeal airways?
Unconscious pts
No gag reflex pts
When do you use a nasopharyngeal airway?
Conscious, semiconscious, or unconscious pts with or without gag flex
When should you proceed with an advanced airway?
Difficult to bag mask vent
Airway compromise
Need to isolate airway
What should you use to monitor ET tube?
Waveform capnography
If waveform capnography jumps up, it may indicate...
ROSC
If a patient is in cardiac arrest what are the first two steps?
(1) CPR
(2) Attach AED
What rhythms are shockable?
VFib or pulseless VTach
What rhythms are NOT shockable
Asystole or PEA
How often should you give epinephrine?
Every 3-5 minutes
When should you consider giving amiodarone?
After you have given 3 shocks and 3 CPR sessions and they are still in VF or pVT
When should you determine if the rhythm is shockable for asystole or PEA in the cardiac arrest algorithm?
After the first CPR session (2 minutes)
When should you start treating reversible causes of asystole or PEA?
After the second CPR session
Bradycardia is categorized as a HR less than...
50
When should you give atropine?
When there is bradycardia and perfusion is low
If atropine fails in treating bradycardia, what should you do?
(1) Transcutaneous pacing
(2) Dopamine
(3) Epinephrine
If atropine, tcp, dopamine, epinephrine all fail to tx bradycardia, what should you do?
(1) Seek expert consultation
(2) Transcutaneous pacing
When should you use synchronized cardioversion in tachycardia?
If the pt is hemodynamically unstable
What should you do if you encounter a pt who has a pulseless tachycardia?
Manage it like a cardiac arrest algorithm
Most symptomatic tachycardias will present with a HR of greater than
150
If a tachycardia patient is hemodynamically stable, what is the next thing you should assess?
If QRS is wide (>= 0.120 sec)
If QRS is not wide for a tachycardia patient, what should you do next?
(1) Vagal manuevers
(2) Adenosine
(3) Bblock or CCB
(4) Expert consultation
What things do you need to do after ROSC?
(1) Optimize ventilation and oxygenation
(2) Treat Hypotension
(3) EKG
(4) See if pt follows commands
During post ROSC, what things do you need to do to optimize ventilation and oxygenation?
- O2 > 94%
- Advanced airway + capnography
- Don't hyperventilate
During post ROSC, if a pt cannot follow commands, what do you need to do?
Initiate targeted temperature management
If a patient is responsive and talking, what is the next step of the ACS algorithm?
Obtain a 12 lead ECG
What is the dosing of nitroglycerin according to the ACS algorithm?
Every 3-5 minutes for a maximum of 3 doses
What are the contraindications of nitroglycerin according to the ACS algorithm?
- Severe bradycardia
- Tachycardia
- Hypotension
- Phosphodiesterase inhibitors
Initiation of fibrinolytic therapy, if appropriate, within _____ of hospital arrival and ______ from onset of symptoms
Initiation of fibrinolytic therapy, if appropriate, within 1 hour of hospital arrival and 3 hours from onset of symptoms
In ACS algorithm, what determines whether or not a STEMI gets reperfusion or not?
Whether or not the sxs of onset are less than 12 hrs