2mo infant is exclusively breastfed. What nutritional supplement?
Oral VitD to prevent rickets
What HTN drug causes peripheral edema, flushing, dizziness?
CCB eg nifedipine
15yo girl with recurrent candida infections of skin and mucous membranes since childhood. Dx?
Chronic mucocutaneous candidiasis (T cell dysfunction)
57yoM with impotence for 1 year rand bronze colored skin. Ferritin concentration is 4050 NG/ml. Increased risk for what complication?
1. Liver (primary organ)--hepatocellular carcinoma
2. Others: pancreas (DM), heart (CHF), skin, thyroid (hypo), gonads, joints (arthritis)
87yo's daughter: "we want my mother to receive hospice care at home but no one wants her to die at home. Can she still have hospice services?"
Yes. Hospice can provide home based care and attempt to transfer the pt to another site before death.
32yoF with 4d of fever with lymphatic obstruction. PE: the left lower extremity is diffuse lay red and edematous from just below the knee to the ankle, with a sharp demarcation separating the erythematous area from the normal skin at the knee. The erythematous area is painful and hyperesthetic to touch. The left oral nodes are enlarged and painful. Dx and cause?
Erysipelas
- usually caused by group A strep
- Tx: IM or oral penicillin/erythromycin
16yo girl with painful genital lesions or 2d. Lots of sexual partners. Exam shows two 3x3mm ulcerated lesions on the anterior vaginal vault. How prevent transmission with new partner?
Consistent condom use (NOT pharmacological treatment)
37yo primigravid at 25 weeks' gestation with confusion for 12 hours. Fever and intermittent nausea and vomiting over the past 2 weeks. No contractions, but decreased fetal movement. Family Hx of T1DM, seizure disorder. T 38.8, P 168/min, BP 187/84. Mildly enlarged thyroid gland. Lungs clear. 3/6 systolic ejection murmur. Fetal heart rate 182/min. Labs show: Hb 9.9, platelets 282k, Serum: Na 134, Cl 94, K 2.9, Thyroid-stimulating hormone 0.01, AST 33, LDH 112, Uric acid 5.4. Dx?
Thyroid storm
- Precipitants: infection, DKA, stress (childbirth, trauma, surgery, illness)
- Sx: fever, tachycardia, agitation, confusion, GI symptoms (n/v/d)
- Tx: supportive therapy with IV fluids, cooling blankets, glucose; PTU ever y2h, follow with iodine; beta blockers to control HR; dexamethasone to impair t3 from T4
37yo F with 4-month history of numbness, burning, and tingling of the toes and soles of her feet. 3-year hx of recurrent mouth sores. Numerous oral apthous ulcers, genital ulcers, and several 2.5-cm red lesions over the left anterior tibial region. Photophobia. Ankle reflexes are absent. Proprioception and sensation to pinprick and vibration decreased in lower ext. Dx?
Behcet syndrome
- autoimmune vasculititc disease
- Sx: recurrent oral and genital ulcerations (usu painful), arthritis (knees, ankles), eye involvement (uveitis, optic neuritis, conjuncitivitis), CNS involvement (intracranial HTN, meningoencephalitis), fever, wt loss; erythema nodosum-like lesions, pseudofolliculitis
- Dx: bx
Tx: steroids
*NOT polyarteritis nodosa
- can be associated with hep B, HIV, drug reactions
- Sx: fever, wt loss, myalgias, abdominal pain (bowel angina)
- Dx: bx; elevated ESR and pANCA
- Tx: corticosteroids (if severe, cyclophosphamide)
87yo F with fever for 1 day. Urinary catheter was placed 2 weeks ago. Has dementia, Alzheimer type, and is unable to communicate verbally. T 37.8 C, P 86/min, BP 120/74. Mucous membranes are moist and pink. Urinalysis shows: Color cloudy brown, Ph 8.8, Blood 2+, Glucose negative, Protein 2+, RBC numerous, wbc 20-25, Nitrites 3+, leuk esterase 3+, bacteria many. Gram stain shows gram-negative bacilli. Which would have prevented?
Use of incontinence briefs instead of the catheter (NOT changing catheter daily)
32yo M with AIDS with 1-week history of T to 40 C and cough. Current medications include trimethopim-sulfamethoxazole and three antiretroviral agents. Moist crackles over right lung base. X-ray of the chest shows an infiltrate in the right lower lobe. Causal org?
Stretococcus pneumoniae (NOT Pneumocystitis jiroveci b/c taking prophylactic oral bactrim)
77yo F with lesions on her left arm for the past 2 months. Underwent modified radical mastectomy of the left breast for breast cancer 20 years ago complicated by chronic edema of the LUE. Two r-mm, raised, hard, purple lesions just above the left elbow. Dx?
Lymphangiosarcoma
- rare malignant tumor which occurs in long-standing cases of primary or secondary lymphedema. It involves either the upper or lower lymphedematous extremities but is most common in upper extremities.
57yo F with 2-week history of progressive jaundice and a 5-kg weight loss. Dark urine and pale stools. No meds. BP 120/80. Gallbladder palpated in the RUQ. Urine dipstick is positive for bilirubin. Ultrasonography shows a dilated gallbladder and dilated intrahepatic and extrahepatic biliary ducts. No calculi. Next step?
CT scan of the abdomen (Obstructive jaundice due to carcinoma head of pancreas)
- Courvoisier's sign: palpably enlarged gallbladder which is nontender and accompanied with mild painless jaundice, the cause is unlikely to be gallstones.
(NOT Lap Cholecystectomy)
One hour after splenectomy, 42yo M has severe shortness of breath. Additional injuries include left rib and pelvic fractures. T 36.3, P 133/min, BP 80/60. Breath sounds are absent on the left. Bowel sounds are absent. Next step?
Needle thoracostomy (pneumothorax; severe)
NOT CXR
67yo M with alcoholism. 15-year history of poorly controlled hypertension; takes hydrochlorothiazide, not compliant. BP 170/102. Funduscopic examination shows arteriovenous nicking and tortuosity of the arteries. Risk for?
MI
- hypertensive retinopathy: AV nicking and tortuosity of the arteries
NOT subarachnoid hemorrhage
32 year old woman with 1 month of diarrhea, 8lb weight loss, three to four semiliquid stools daily. No fever, abdo pain or rectal bleeding. Just returned from scuba diving in Mexico 6 weeks ago. Boyfriend is symptom free. Abdo and rectal exam are normal. What is organism?
Giardia lamblia
NOT V cholerae (up to 15 stools per day)
37yo F from Guatemala with joint pain, swelling, and stiffness of her wrists and hands for 2 years. Ibupforen ineffective. No fever, cough, or weight lossl. Received all immunizations. BMI 20. Spleen tip is nontender and is palpated 4 cm below left costal margin. Grip strength is decreased. Labs: Hb 10, Leukocyte count 2.5k, Platelets 125k. Cause of the leukopenia?
Felty syndrome
- disorder that involves rheumatoid arthritis, a swollen spleen, decreased white blood cell count, and repeated infections. It is rare.
37 yr old woman, sudden onset fever 7 days after splenectomy for ITP. T 102.4, mild distension and diffuse tenderness, no rebound, rigidity or guarding. No bowel sounds. Labs hg 9.8 Leuks 21,300 Platelet 105, 000, amylase 124. chest xray shows left pleural effusion. what is the most likely cause of the findings?
subphrenic abscess (Post-splenectomy subphrenic abscess, phrenic nerve impingement cause refered shoulder pain, abscess fits the Fever, Increase Leukocyte count)
NOT pneumonia
3yo girl with fever and ear pain for 1 day. Has had clear nasal discharge and cough for 3 days. History of several ear infections and one episode of streptococcal pharyngitis over the past 12 months. Father smokes in the house, family has two cats. Swims frequently. T 38.5, P 110/min, BP 80/50. Clear nasal discharge, erythema and bulging of the right tympanic membrane, and erythema of the throat without exude. Recommendation to prevent recurrence?
Avoidance of passive smoke exposure
62yo M with fatigue for 9 weeks. Drinks moonshine. HCT 29%, MCV 78, and mean corpuscular hemoglobin concentration is 25%. Blood smear shows hypochromic, microcytic erythrocytes and normochromic, normocytic erythrocytes. Bone marrow shows greater than 10% normoblasts containing iron-laden mitochondria that surround the nucleus and appear as rings on Prussian blue staining. Iron and transferrin saturation increased. Cause?
Sideroblastic anemia
- caused by abnormality in RBC iron metabolism
- hereditary or acq (drugs eg INH, alcohol, chloramphenicol; exposure to lead; neoplastic disease)
- Labs: increased serum iron and ferritin, normal TIBC, ringed sideroblasts in bone marrow
- Tx: remove offending agents; consider pyridoxine
NOT hemochromatosis
30yo F routine exam. 10-year history of type 1 diabetes mellitus. Microalbuminuria, her hemoglobin A1c is 7%, and serum Cr is 1.8. Intervention?
Administration of an angiotensin-converting enzyme (ACE) inhibitor
NOT inc dose of insulin
19yo F at 32 weeks' gestation with 1-month history of a generalized rash that has not expanded or changed. No pruritis or fever. No prenatal care. Macular rash involving the palms, chest, back, abdomen, extremities, and soles. Causal oragnism?
Treponema pallidum
NOT Rubella:
"You drive CARS with your palms and soles"
CA- Coxsackievirus A
R- Rickettsia Rickettsii
S- Syphilis (secondary)
22yo F with asthma. Treated for six acute episodes of wheezing and nonproductive cough during the past year. Last episode 1 mo ago. Sx exacerbated when outside during the spring and fall. On albuterol inhaler. Smoked daily for 5 years. X-ray of the chest normal. Which will reduce frequency of exacerbations?
- Fluticasone inhaler therapy
(Not influenza vaccine)
6 month old boy, chronic constipation since the age of 1 week. Current Rx with rectal stimulation, glycerin suppositories, and 4 ounces of prune juice produces string-like stool every 4 days. No vomiting. Growth and development are appropriate for age. Abdominal exam shows distension, no tenderness. Rectal exam, no palpable stool in ampulla. What is next step in mangement?
Rectal manometry
- Hirshsprung disease: Chronic progressive constipation with onset in infancy + abdominal distension + empty rectum
37yo M with 6-week history of the rash shown. Similar rash over the past 5 years resolved with Rx. Sun exposure, the rash becomes lighter than his tanned skin. Pharmacotherapy?
Selenium sulfide shampoo
- tinea versicolor (pityriasis versicolor) fungal infection
82yo M with shortness of breath at rest, increasing malaise, generalized weakness, and depressed mood for 6 weeks. Bruises easily and has bleeding and inflammation of the gums. Hypertrophic, lichenified patches over the upper extremities. No memory loss. Dx?
- Vitamin C deficiency
(Scurvy, malnutrition, easy bruising, bleeding gums)
62yo M 4 hours after sudden onset of vomiting and sever abdominal pain. Has had mild, intermittent epigastric pain, relieved with antacid use. No hx of serious illness. Smoked daily for 35 years. Appears diaphoretic and is in acute distress. T 38.4 C, P 100/min, BP 115/75. Bowel sounds are absent. Next step?
X-rays of the chest and abdomen (to visualize perforation)
NOT CT abdomen
2yo girl with shortness of breath for the past 2 hours. 3-day history of runny nose, sneezing, and nasal congestion. T 38.5 C, p 130/min, rr 48/min. Dyspnea. Stridor and moderate retractions with inspiration. Lungs clear. Barking cough. Causal organism?
Parainfluenza virus
NOT Bordetella pertussis !!!
42yo F with decreased energy, apathy, and difficulty sleeping since being fired from her job 3 weeks ago. Crying spells, weight loss, tearful. Speech is soft and goal directed. Not thought abot suicide and does not want to die. Labs normal. Next step?
Citalopram therapy (SSRI)
NOT psychodynamic psychothreapy (Psychodynamic therapy, also known as insight-oriented therapy, focuses on unconscious processes as they are manifested in a person's present behavior. The goals of psychodynamic therapy are a client's self-awareness and understanding of the influence of the past on present behavior.)
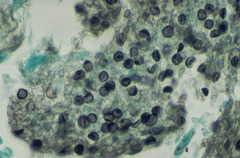
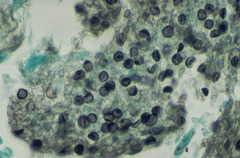
25yo F with AIDS comes with 10-day history of fever, shortness of breath, night sweats, and a nonproductive cough. T 38.6. CXR with bilateral interstitial infiltrates. Silver stain positive for cysts and organisms. pharm?
Trimethoprim-sulfamethoxazole
- diagnosis of Pneumocystis carinii (jirovecii) pneumonia is to perform a Gomori methenamine silver (GMS) stain on the lung tissue or bronchoalveolar lavage (BAL) fluid. The cyst wall is stained, and the organisms appear as crushed ping-pong balls
37 yo man restrained driver in a car with no airbags. Steering wheel was deformed. En route, his hemodynamic status and respirations were stable. He has severe anterior chest pain. P110, RR 24, BP 90/60. Exam shows jugular venous distention (JVD), tenderness of the sternum to palpation. Breath sounds are equal. Heart sounds are decreased. Upper and lower extremities are normal. After 2L 0.9% saline, pulse decreases to 100/min, BP increases to 100/70. In the next 10 min, BP drops to 80/50. Which explains changes in BP?
Pericardial tamponade (hypotension, JVD)
NOT ruptured thoracic aorta
14yo girl 6 hours after onset of severe abdominal pain. Hx of similar episodes and swelling of her arms and legs since early childhood. Associated with swelling of the lips and eyes and have not responded to rx with hydroxyzine. VSS. Rigid and diffusely tender abdomen. Bowel sounds are increased. Substance that is most likely decreased?
C1 esterase inhibitor
- Hereditary angioedema (recurrent attacks of intense, massive, localized subcutaneous edema involving the extremities, genitalia, face, or trunk, or submucosal edema of upper airway or bowels)
27yo F 25 minutes after MVC. Restrained driver. Upper abdominal and left-sided chest pain. P 120/min, rr 18, BP 80/50. Tenderness over the left costal margin and LUQ of abdomen. X-ray of the chest shows multiple fractures of the ribs. BP stabilizes after 2 L lactated Ringer solution. Next step?
CT scan of the abdomen
NOT contrast angiography
4yo boy with increasing left ear pain for 2 weeks. T 38.5. Erythematous, bulging tympanic membrane an an edematous auditory canal with a small amount of mucopurulent dischage. Ear displaced laterally. 1-cm, freely moile, nontender mass palpated over the left anterior neck. Next step?
CT scan of the temporal bone (mastoiditis)
- NOT oral amoxicillin
47yo M with 2-year history of increasing left knee pain. Over the past 6 months, he has been awakening at night with pain. Pain exacerbated with walking and prolonged standing. Stoped participating in spots. At age 16, he sustained fractures of the left proximal tibia while playing football and undeerwent ORIF. No locking or catching. Varus deformity of the left knee. Explanation?
Post-traumatic arthritis
NOT nonunion of his prior fracture
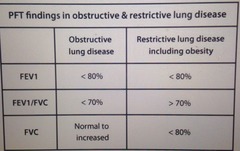
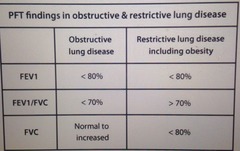
#PFTs in restrictive vs obstructive lung disease
#37yo M with fever, generalized muscle aches, and an ulcer on his neck, began 10 days ago as a painless, itchy papule that enlarged over a 2-day period, until small, fluid-filled blisters formed on top of the papule. Painless ulcer covered by a black scap. Emplyed as a postal worker and works part-time as a horticulturist. No travel. Eschar-covered ulcer surrounded by nonpitting edema. Dx?
Cutaneous anthrax
#what causes urinary incontinence of normal pressure hydrocephalus?
failure to inhibit the voiding complex
#what is the underlying cause of slipped capital femoral epiphysis?
disruption of the femoral head epiphyseal plate
#37yo F with increasingly severe pain and masses in both breasts over the past 3 months. 12-year hx of similar episodes. Masses vary with menstrual cycles. Used OCP for 16 years. Multonodular breasts. No axillary adenopathy. Dx?
Fibrocystic changes of the breast
#Indications for cone biopsy of cervix
- The abnormal tissue cannot be seen with colposcopy but was found in cells collected from a biopsy of the cervical canal
- the abnormal tissue seen with colposcopy extends high into the cervical canal. A cone biopsy is done to remove and examine the abnormal tissue.
- Cervical cancer is suspected based on Pap test results, colposcopy, and cervical biopsy. A cone biopsy can determine the extent, depth, and severity of the cancerous tissue and can guide treatment decisions.
#Is haloperidol contraindicated in pregnancy?
No
#How does Crohn's cause small bowel obstruction?
small bowel fibrotic stricture
#What are the causes of diabetes insipidus?
1. Central DI
- idiopathic
- trauma: surgery, head trauma*
- other destructive processes involving the hypothalamus: tumors, sarcoidosis, TB, syphilis, encephalitis
2. Nephrogenic DI
- chronic Li use
- other causes: hypercalcemia, pyelonephritis, demeclocycline use, congenital
#3mo infant with tachypnea and tachycardia for 10 days; during this period he has been feeding poorly. grade 3/6 holosystolic murmur and a grade 2/6, apical mid-diastolic murmur are heard. X-ray of the chest shows cardiomegaly with increased pulmonary vascular markins. Echocardiography shows a large ventricular septal defect. Cause?
Excessive pulmonary blood flow
#echo of endometrioma
low level, homogeneous, internal echos
#22yo F with acute myelogenous leukemia undergoes evaluation prior to discharge. Has received induction chemotherapy and transfusions via a subcutaneous central venous catheter for the past 4 weeks. Two days ago, CBC and bone marrow biopsy were normal. Most appropriate recommndation to avoid complications?
Hand washing with an antibacterial soap prior to contact with the catheter
#lab findings of DKA
- hyperglycemia: serum glucose > 450mg/dl and <850 mg/dl
- metabolic acidosis
- ketonemia and ketonuria
- hyperosmolarity
- hyponatremia
- potassium: hyperkalemia but total body K low
#how to manage molar pregnancy?
suction curettage
#how to manage superficial thrombophlebitis?
application of warm compresses
# 25yo F with shortness of breath, marked malaise, weakness, and fatigue for 4 hours. Developed muscle soreness after an unusually streneous physical workout; took ibuprofen 1 hour prior. Hx of frequent migraines Rx with metoprolol. Facial flushing and mild periorbital edema. Multiple wheezes throughout lung fields. Avoidance of which to prevent recurrence?
aspirin
#47 yo M at follow-up after being diagnosed with stage I HTN 5 months ago. Started on hydrochlorothiazide. Over the last month, he has felt fatigued. Exam is normal. Which is causing his symptoms?
hypokalemia
#32yo F ith 2-day history of fever and an area of swelling and redness on her right forearm. No travel, no hx of trauma. Epitrochlear lymph nodes are enlarged. Distal radial aspect of the right upper extremity shows an 8 x 12-cm warm, erythematous area of edema that is tender to palpation; warm, tender red streak extending from this area to the elbow. Causal organism?
beta hemolytic streptococcus
- lymphangitis caused by strep pyogenes( beta hemolytic strep )
#52yo F with 8-month hx of intermittent nonproductive cough. No meds. Smoked daily for 25 years. Sinusitis over 18 months. Pale nasal mucosa and cobblestoning of the posterior pharynx. Lungs clear. No clubbing or cyanosis. Cause?
allergic rhinitis
#what does granulosa cell tumor produce? Sertoli-Leydig cell tumor? dysgerminoma?
estrogen; testosterone ; hypercalcemia
#47yo F with intermittent palpitations over the past 3 weeks. No smoke and no meds. Consumes two caffeinated beverages daily and does not drink alcohol. X-ray of the chest shows bilateral hilar adenopathy and clear lung fields. ECG shows first-degree atrioventricular block. Dx?
Sarcoidosis
#42yo F in ED 30 minutes after found unconscious in her bed. 6-year history of systemic lupus erythematosus treated with prednisone. Been on a drinking binge and not eating. Three days ago, had rhinitis, conjunctivitis, and a nonproductive cough. T 38.9 P 110/min, palpable SBP is 80. Initial step?
Corticosteroid therapy
# 5yo boy with 1-week history of a sore throat and a 1-day hx of dark urine. Positive rapid streptococcal test 4 days ago and has received penicillin since. T 37. Urine: glucose negative, protein 3+, ketones negative, RBC too numerous. Substance that is most likely decreased?
C3
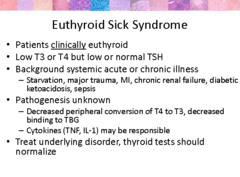
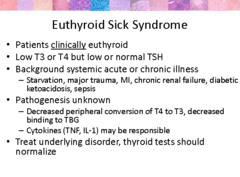
#euthyroid sick syndrome
Euthyroid sick syndrome can be described as abnormal findings on thyroid function tests that occur in the setting of a nonthyroidal illness (NTI), without preexisting hypothalamic-pituitary and thyroid gland dysfunction. After recovery from an NTI, these thyroid function test result abnormalities should be completely reversible.
#when to give HIV prophylaxis?
1. Pneumocystic pneumonia CD4<200 (bactrim)
2. Mycobacterium avium CD4<100 (clarithromycin and azithromycin)
3. Toxoplasmosis CD4<100 (batrim)
4. TB: yearly PPD test
#27yo M and wife unable to conceive over the past 4 years. Left testicle drags. Both testes are well descended. Left scrotum hangs lower than the right, and there is a soft tissue mass near the top of the left testes that feels like a bag of worms. In the supine position, the mass mostly dissapears. Dx?
varicocele
1. 77yo F with 2-day hx of cramping abdominal pain, distension, N/V. T 99.4, BP 110/86, P 112, R 24/min. Cardiopulmonary exam wnl. Bowel sounds are High-pitched, abd xr shows air-fluid levels throughout small bowel and air in the liver; no gas in colon or free air. Dx?
Gallstone ileus
- gallstone enters bowel lumen via cholecystoenteric fistula--gets stuck in terminal ileum and causes obstruction
2. 32yo F with lethargy and boredom since birth of her son 5 months ago. Worries about her ability to care for him and has had frequent palpitations. Unable to sleep after nighttime feedings. Stopped breastfeeing 1 month ago. Son is healthy and wnl. VSS. Remembers 1/3 objects after 5 minutes. Serum cholesterol is 265. Next step is measurement of which of the following serum concentrations?
TSH
(Some breastfeeding mothers with hypothyroidism struggle to make a full milk supply. )
3. 52yo F with decreased libido; this sx began 8 mo ago after TAH-BSO for leiomyomata uteri and menorrhagia. Taking HRT with conjugated estrogen since surgery. Exam shows moist, rugated vagina. Cause?
Decreased androgens
- Decrease testost due to oophoreectomy ,decrease androstenedione and Dhea.
Post menopuasal women, Estrogen replacement therapy, moist rugated vagina, suggest increase Estrogen........> increase sex hormone binding globulin which in turn decrease availability of testost and may exacerbate sign of androgen loss ( decrease libido).
4. 82yo F with 6-week Hx of increasing forgetfulness. Left the stove on when she went to bed, difficulty remembering past events and seems unconcerned about her memory lapses. Hx of similar symptoms 2 and 5 years ago that were successfully treated with medication. Psychomotor retardation, flat affect =, trouble repeating three numbers in sequence. BUN 25, Cr 1.7. Dx?
Major depressive disorder
5. 20-mo girl with fever and cough for 2 days. Has had several similar episodes since the age of 4 months. 25th %ile for length and 5th %ile for weight. T 38 C, P 150/min. Mild clubbing. Wheezing and bilateral crackles are heard at the lung bases. CXR shows streaky densities bilaterally with mild hyperinflation. Dx?
Cystic fibrosis
-failure to thrive (small stature and low weight) with pulmonary disease and repeated pulmonary infections
NOT alpha1 antitrypsin deficiency (emphysema later in life as an adult)
6. 16yo boy with fever and cough with right-sided chest pain for 2 weeks. Visited grandparents in Albania for 2 weeks. Thin, pale, T 38.2 C, P 76/min. Shallow respirations with decreased breath sounds at the right lung base. CXR shows right pleural effusion and hilar adenopathy. Dx?
Pulmonary tuberculosis
*hilar adenopathy
NOT pulmonary aspergillosis
7. 67yo M in ED 1 hour after onset of vertigo, nausea, and imbalance. 20yr Hx of HTN, BP 210/115. Small right pupil, mild right ptosis, and nystagmus. Weakness of the right palate. Sensation to pinprick decreased over right side of face and left extremities. Incoordination on finger-nose testing and heel-knee-shin testing on the right. Artery occluded?
Right vertebral
Carotid and vertebral artery dissection: partial horner's (ptosis, miosis but no anhydrosis) with head or neck pain
8. 6-mo F with poor feeding and labored breathing for 2 months. Recurrent respiratory tract infections since birth. to-and-fro murmur in second left intercostal space, a loud S2, bounding peripheral pulses, widened pulse pressure. Dx?
Patent ductus arteriosus
9. 52yo M with hiccups for 1 week. Smoked two packs daily for 30 years. No alcohol. T 37C, BP 150/95, P 70/min, resp 12/min. Sodium concentration is 120. X-ray of the chest shows right hilar mass. Next step?
Fluid restriction
(SIADH from small cell lung CA)
10. 67yo M in ED 4 hours after severe midlumbar back pain. Anxious, pale, diaphoretic. T 37.1, BP 105/65, p 120/min. XR of lumbar spine show degenerative disc disease with calcifications anterior to the vertebral bodies. Dx?
Ruptured aortic aneurysm
NOT aortoiliac occlusion
11. 4yo boy with 3-day history of fever, cough, and runny nose. No wheezing, vomiting, or diarrhea. At the 75th percentile for height and 10th percentile for weight. T37.5 C, Capillary refill time is 2 seconds. Exam shows clear rhinorrhea. Cardiac exam in "Media Player." Dx?
Upper respiratory tract infection
NOT ALWAYS HEART DISEASE EVEN IF MEDIA PLAYER RESULT
12. 44-yo F G4P4 with 9-month history of progressive loss of small amounts of urine while running; she now has to wear an absorbent pad. Second-degree cystourethrocele. Dx?
Stress incontinence
A cystourethrocele, or prolapsed bladder with urethra, is a bulging of the bladder and urethra into the vagina
13. 27yo F with 2-day history of weakness of her arms and legs and numbness of her hands and feet and 4-hour hx of mild shortness of breath. Sensation of "electrical shocks" extending from the buttocks to the feet. Today, she tripped and fell several times and was unable to button clothes or hold utensils. Three weeks ago, had mild upper gastrointestinal illness that resolved. Mild facial weakness; cranial nerves are otherwise intact. Babinski's sign is absent bilaterally. Sensation to vibration is slightly decreased at the fingers and toes. Most appropriate test to establish cause?
Electromyography and nerve conduction studies
- Guillain Barre syndrome dx: CSF analysis (elevated protein but normal cell count), electrodiagnostic studies (decreased motor nerve conduction velocity)
- Tx: IV immunoglobulin if significant weakness; if progression continues, plasmapheresis
14. Newborn is in severe respiratory distress following delivery. Born at 35 weeks' to a 35yo F G2P1A1 who did not receive prenatal care. Pallor with perioral cyanosis, anisarca, hepatosplenomegaly, and scattered petechiae. Cord blood Hb is 4, and reticulocyte count is 18%. Direct antiglobulin (Coombs') test is positive. Which set of blood groups?
Mother: O, Rh-negative; Newborn O, Rh-positive
(Rh factor)
15. 32yo F with vaginal discharge for 2 weeks. Sexually active with one female partner for 5 years. Last pap 6 years ago. No drugs or alcohol. Exam shows grayish vaginal discharge with a pH greater than 4.5 Wet mount will show which?
Clue cells
16. 72yo M with hypertension had increasingly severe back pain over the past 2 months. Had a myocardial infarction 4 years ago. Marked tenderness over T11, T12, L1, and L2. X-ray of lumbosacral spine shows osteoblastic lesions. Dx?
Metastatic prostate carcinoma
17. 50yo F with progressive dyspnea over the past 2 weeks and constant, sharp chest pain for 4 days. Pain localized to center of chest and worse while supine. Underwent right, modified radical mastectomy and adjuvant chemo. Hx of hypothyroidism Rx with thyroid replacement therapy. Smoked one pack of cigarettes daily for 30 years. Dyspneic and diaphoretic. T 37.2, BP 90/70 with pulsus paradoxus of 20 mm Hg. Pulse is 110/min. Jugular venous distention to angle of mandible. Liver is 14 cm with 4 cm of shifting abdominal dullness. ABG on room air shows: pH 7.5, PcO2 30, PO2 70. CXR shows enlarged cardiac silhouette with a globular configurtion. ECG shows sinus tach with nonspecific ST-seg changes. Next step?
Echocardiography (diagnostic)
NOT paracentesis (pericardiocentesis) only if not hemodynamically stable nonhemorrhagic tamponade
18. County health officer investigates outbreak of illness among persons ttending a church picnic. Onset of nausea and vomiting 3 to 4 hours after the picnic. Investigation implicates egg salad as the vehicle of transmission. Cause?
Staphylococcus aureus
Foods that are associated with staphfood poisoning include:
Meats.
Poultry and egg products.
Salads such as egg, tuna, chicken, potato, and macaroni.
Bakery products such as cream-filled pastries, cream pies, and chocolate eclairs.
Sandwich fillings.
Milk and dairy products.
Sx include nausea, vomiting, retching, stomach cramping, and diarrhea
NOT
Beef, poultry, milk, and eggs are most often infected with salmonella
19. 67yo M with 3-day histor of fever and headache. Five years ago, he underwent placement of a mechanical aortic valve for treatment of sequelae of rheumatic fever. T 40 C, BP 110/65, P 110/min. 3/6, systolic ejection murmur is heard. Neuro examination shows mild left hemiparesis. Babinski's sign is present on the left. Greatest risk for which complications?
Brain abscess
NOT
-Fever and headache are not features of embolic stroke
20. 5yo girl with T 40C, tachypnea, and a nonproductive cough for 12 days. Four days ago was treated with antibiotic for suspected pneumococcal pneumonia. Diminished breath sounds over the right lower lung fields and dullness to percussion at the right costphrenic angle. Dx?
Empyema
Empyema is defined as pus in the pleural space. It typically is a complication of pneumonia.
A lung abscess is a subacute infection in which an area of necrosis forms in the lung parenchyma. It usually is in a dependent section of the lung, more often involves the right lung than the left, and is most commonly seen after aspiration of oropharyngeal secretions. Lung abscesses have a slow, insidious presentation and usually develop 1-2 weeks after the initial aspiration event.
21. 37yo primigravid woman at 9 weeks' gestation with progressive nausea and vomiting. Sx began at 6 weeks' but have worsened. T 36.9, P 105/min, BP 110/60. Serum electrolyte concentrations are wnl. U/A shows 3+ ketones. In addition to intravenous hydration, most appropriate initial step?
Antiemetic therapy
22. 72yo M with 2-month history of urination twice nightly, frequency, and urgency. 15-year hx of T2DM. BP 135/86. Mild enlargement of the prostate with no palpable nodules. His postvoid residual volume is 10 mL. Urea nitrogen concentration of 45 mg/dL and creatinine concentration of 3.8 mg/dL. Urine dipstick shows 3_ prtein. Whihch would have prevented progression of renal disease?
Oral enalapril therapy
23. 4-week-old newborn with increasing difficulty feeding, poor weight gain, and excessive perspiration since birth. Respirations are 80/min and labored. A grade 2/6 holosystolic murmur is heard over the lower left sternal border. Lungs are clear. Chest x-ray shows cardiomegaly with increased pulmonary vascular markings. ECG shows right ventricular hypertrophy. Explanation for absence of murmur on initial exam?
High pulmonary vascular resistance
VSD murmurs can arise from lower muscular part or upper membranous part. Lower muscular ones heal on their own and dont give much problem. Upper portion defects stay on for long and do give the particular holosystolic murmur described in the question stem. The murmur is not heard just after birth at the initial exam, reason being the pulmonary vascular resistance is too high and lungs are not totally functional. So No blood is flowing through the pulmonary system until high oxygen later on after birth shuts down the PDA and loosens up the pulm vasc resistance.
24. 62yo F with 2-day history of fatigue and a 1-hour hx of headache and confusion. No fever, nausea, or vomiting. 6-year hx of HTN treated with hydrochlorothiazide and lisinopril. BP 250/135. Funduscopic exam shows bilateral papilledema. Lungs clear. S4 and no murmurs. ECG shows left ventricular hypertrophy with a strain pattern. Initial pharmacotherapy?
Nitroprusside
Papilledema indicates malignant HTN. Tx is with IV labetalol, nitroprrusside or nicardipine.
NOT hydralazine or nifedipine
25. 16yo boy with neurofibromatosis with 1-year history of headaches during which his parents say he appears pale. Six months ago, operative treatment for optic nerve glioma. BP 164/105, P 102/min. Thyroid glands are not enlarged. No murmurs. Cause of high blood pressure?
Catecholamine-producing tumor
Dx is MEN III (also called MEN IIb); it is caracterized by medullary CA of the thyroid (even though the gland is not enlarge), pheocromocytoma and mucocutaneous neuromas (neurofibromatosis, tuberous sclerosis are mucocutaneous diseases).
26. 18yo M 1 week after he had a BP 140/110 during routine precollege examination. Upper extremities appear to be more muscular than the lower extremities. Radial pulses are normal; femoral, posterior tibial , and dorsalis pedis pulses are decreased. 2/6 systolic murmur heard over the precordium, anterior chest, and back. ECG shows left ventricular hypertrophy. Next step?
Operative treatment
(surgical decompression)
- coarctation of the aorta
27. 15yo boy 30 minutes after a 2-minute episode of loss of consciousness after completing a 400-meter race. Feels fine except for shortness of breath. BP 110/70, P 70/min. Lungs are clear. 2/6 systolic murmur is heard at the left sternal border with minimal radiation to the neck, the murmur becomes louder when he stands. Dx?
Hypertrophic obstructive cardiomyopathy
28. Study to compare effectiveness of lorazepam and midazolam in providing sedation for children who require mechanical ventilation. 100 kids ramondly selected. Paralytic agents are administered to 26 of the 50 children in the lorazepam group and to 2 of the 50 children in the midazolam group to allow more synchronized mechanical ventilation. Results show sedation score of 1 for 92% of the lorazepam group and 12% of the midazolam group. Which features of this study raises concern of validity?
Confounding variables
# Previously healthy 10yo boy with 2-day hx of pruritic rash on arms and legs, 24 hours after played in wooded area. No fever. Pet cat at home. Severe erythema and bullous lesions with discharge; there is a sharp line of demarcation between the rash and the unaffected skin. Pic shown. Recommendation to prevent recurrence?
Avoidance of the wooded area
- poison ivy type IV hypersensitivity
#32yo F w/ 10-day hx of persistent cough keeps her awake at night and worse with physical activity, productive of white sputum in the morning. Sx began w/ URI 10 days ago. Smoked one pack of cigarettes daily for 16 years. Not in distress but has a rasping cough. T 37.4 C, P 78/min, resp 12/min, BP 130/80. No pharyngitis or facial tenderness. Scattered end-expiratory wheezes bilaterally. Peak expiratory flow rate is mildly decreased. CXR wnl. Next step?
Inhaled B2-adrenergic agonist
#benzodiazepine withdrawal symptoms
sleep disturbance, irritability, increased tension and anxiety, panic attacks, hand tremor, sweating, difficulty in concentration, dry wretching and nausea, some weight loss, palpitations, headache, muscular pain and stiffness and a host of perceptual changes
# 20yo M routine health maintenance examination. 15-year hx of difficulty relaxing his hands after tightly gripping objects or after shaking hands. Father has cataracts and frontal baldness. Exam shows thin forearms. Moderate weakness of hands. Dx?
myotonic muscular dystrophy
- classic DM1 have muscle weakness and atrophy, myotonia, cataracts and frequently have cardiac conduction abnormalities. Symptoms usually begin between the ages of 20 and 40, but disease onset can sometimes occur in childhood or after age 40. Distal muscle weakness leading to a gait disturbance and facial muscle weakness are often the first symptom
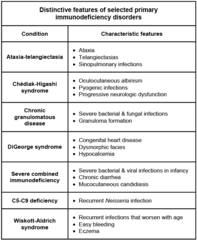
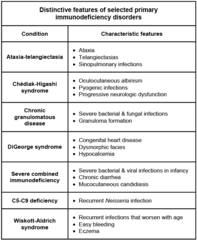
# primary immunodeficiency disorders
# 32yo F with husband unable to conceive for 2 years. Menarche at age of 14 years, Menses irregular 35 - 50 day intervals and last 10 days, not painful. Menstrual flow is normal. No Hx of illness, no meds,. OCPs for 16 years, d/c'd 2 years ago. Husbands sperm count wnl. Patient's BMI is 31. Physical shows acne over face, shoulders, back. TSH, Free testosterone, DHEAS, LH, FSH, all wnl. Dx?
PCOS
- high androgens -> elevated free testosterone
- high androgen and obesity -> estrogen increase
- stimulates LH secretion while inhibiting FSH secretion, leading to an LH to FSH ratio of > 3:1
# 57yo M for routine exam. Smokes 1 pack of cigarettes daily for 37 years. BP 180/112, P 82. Abd exam shows bruit in RUQ and no masses. Hct is 42%, serum urea nitrogen concentration is 23, Cr is 1.4. Cause of bruit?
Accumulation of lipids in the arterial wall
# constrictive pericarditis
Symptoms are often vague and their onset is insidious; they include malaise, fatigue, and decreased exercise tolerance. With progression of constrictive pericarditis, symptoms of right-sided heart failure (eg, peripheral edema, nausea, abdominal discomfort, ascites) become apparent and usually precede signs of left-sided failure (eg, exertional dyspnea, orthopnea, paroxysmal nocturnal dyspnea).
# acute stress disorder vs adjustment disorder with anxiety
- acute stress disorder: PTSD symptoms that last more than 2d but max 1 month ; occur within 1 month of traumatic event
- adjustment disorder: anxiety symptoms less than 6mo
# anovulation vs premature ovarian failure
- anovulation: yes estrogen, no ovulation so no progesterone so irregular periods
- Primary ovarian insufficiency (POI) (premature ovarian failure, premature menopause, or early menopause) is a condition characterized by amenorrhea, hypoestrogenism, and elevated serum gonadotropin levels in women younger than 40 years
# 5mo boy born at 37 weeks' gestation has had persistent wheezing since birth despite rx with nebulized and oral bronchodilators and oral corticosteroids. Diet consists of 32 ounces of iron-fortified cow's milk-based formula daily. Appears nourished and happy. Moderate relief of wheezing with extension of the neck. Mechanism of wheezing?
Compression of the airway by a vascular ring
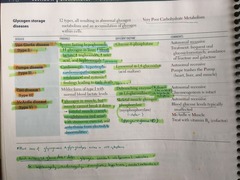
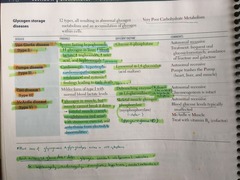
# glycogen storage diseases
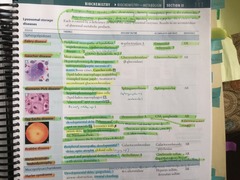
# Lysosomal storage diseases
#13yo girl. Menses have occurred every other month since menarche 10 months ago. LMP 1 week ago. Not sexually active. Development is Tanner stage 3. Next step?
Discussion of pregnancy prevention
#vomiting causes what electrolyte imbalance
hypochloric hypokalemic metabolic alkalosis
#52yo Cantonese woman with husband and brother for follow-up 7 days after removal of a 10-cm complex, solid, cystic adnexal mass. Patient insists to disclose results only to her husband and not to her or to other family members. Appropriate course?
Share the results with the husband only
# 2yo boy with fever and cough for 2 days. Streptococcus pneumoniae meningitis at age of 1 year, bacteremia at 18 months, pnuemonia at 22 months. Two maternal uncles died before age of 2 from "infection." T 39.8. Hb 10, WBC 36k (PMN 70%, Bands 20%, lymphocytes 8%, monocytes 2%), Platelets 240k; IgA <5, IgG 30, IgM <5. CXR shows an infiltrate in the left upper lobe. Next step?
Intravenous immunoglobulin infusion
(common variable imunodeficiency ie decrease in IgG, IgM, IgA)
# 64yo F has moderately severe postoperative pain 1 day after a total abdominal hysterectomy and bilateral salpingo-oophorectomy. Most appropriate analgesic?
Patient-controlled intravenous morphine
# 47yo M with fever and chills for 1 day. 20-year history of alcoholism and cirrhosis of the liver. One month ago, he underwent evacuation of a subdural hematoma, post-op course complicated by generalized tonic-clonic seizures; he has been receiving carbamazepine since. Continues to drink. T 38.9, BP 120/80. scleral icterus, ascites, and splenomegaly. Labs: HCT 39%, MCV 102, Leukocyte count 1200 (PMN 6%, eosinophils 1%, basophils 1%, lymphos 80%, monocytes 12%). Platelets 210k. Cause of decreased leukocyte count?
Carbamazepine therapy
# 47yo M threatening to harm a radio announcer he believed was broadcasting his thoughts. Over the past 20 years, has been hospitalized for similar things. past symptoms improved with neuroleptic therapy; after discharge, he discontinued the medication and his symptoms worsened. Pharm?
Haloperidol decanoate
# DiGeorge syndrome
CATCH22:
Cleft palate
Abnormal facies
Thymic aplasia -> T cell def
Cardiac defects
Hypocalcemia due to parathyroid aplasia
*microdeletion at chromosome 22q11
*thymic, parathyroid and cardiac defects
# 24yo F. Menses occur at regular 28-day intervals and last 5 to 6 days. LMP 3 weeks ago. No meds, Bimanual exam shows a c-cm, mildly tender left adnexa. A pregnancy test is negative. Next step?
Repeat examination in 2 weeks
#23yo F G1P1 requesting postcoital contraceptive advice. One day ago, patient's condom broke during sexual intercourse. LMP 2 weeks ago. Pregnancy test is negative. Recommendation?
Oral levonorgestrel now and again in 12 hours
Prostaglandin F2-alpha: One of the prostaglandins, a group of hormone-like substances that participate in a wide range of body functions such as the contraction and relaxation of smooth muscle, the dilation and constriction of blood vessels, control of blood pressure, and modulation of inflammation. It is used for the induction of abortion, for evacuation of the uterus after a missed abortion, and in the treatment of hydatidiform mole
# 6yo boy with progressive visual loss over the past year. Deterioration of his hearing, speech, writing, and intellectual performance. Maternal uncle had similar symptoms. Visual acuity is 20/200 bilaterally. Funduscopic examination shows optic atrophy. Weakness and spasticity of all extremities. DRT are exremely hyperactive. Babinski's sign is present bilaterally. MRI shows marked symmetric white matter disease involving all lobes. Diagnostic studies will show?
An excess of very long chain fatty acids
Adrenoleukodystrophy (ALD)
------------------------------
CNS Degeneration and Adrenal Cortical Insufficiency
X-Linked Recessive
*** Caused by ACCUMULATION OF VERY LONG CHAIN FATTY ACIDS IN NEURAL TISSUE AND ADRENALS due to mutations in the ABCD1 gene coding for the ALD protein.
Symptoms at 5-15 years of age:
* Decreased academic performance
* Behavioral Changes
* Gait abnormality
* Generalized seizures
* Spasticity, contractures, ataxia, swallowing disturbances
* Hypoadrenalism with skin Hyperpigmentation
* Deterioration of *** Hearing, *** Vision and *** Sensation
* Death within 10 years
# One month after uneventful renal transplant for glomerulonephritis, 38yo F with increased serum urea nitrogen and creatinine concentrations; Had been receiving hemodialysis for 3 years. Current meds include cyclosporine and prednisone. Over the past 48 hours, urine output has remained stable. Both renal biopsy and a radionuclide scan confirm acute rejection. Most effective treatment?
Increased dosage of corticosteroids
#72yo M with chronic abdominal pain and headaches for 4 months. More forgetful over the past 6 months. Hx of gout. Smoked one pack daily for 50 years and drinks 10 oz of homemade whiskey daily. No meds. BP 160/98, p 74/min. Mild short-term memory loss and decreased sensation to pinprick in the distal extremities. Has an ataxic gait. Gouty tophi on dorsal aspect of the left elbox. Labs show: HCT 33%, MCV 70, BUN 17, Glucose 90, Cr 2, Uric acid 14. Next step?
Measurement of blood lead concentration
#52yo F with large pimple on her right hand for 2 weeks that has failed to heal. Resides in southwestern USA where she owns a nursery and garden shop. Painless red papule with several nontender subcutaneous nodular lesions above it. Dx?
Sporotrichosis
1) 4mo old brought to ER after an apparent seizure. Pt has vomiting 6 times over the last 2 days, feeding poorly, and sleeping more than usual. Pt is lethargic and afebrile. Anterior fontanel is tense, bilateral retinal hemorrhages. Dx?
Child abuse
NOT brain tumor
* think most common
*CARELESS* 2) 47yo F brought to ER 30 minutes after a MVC, unrestrained driver. Severe neck pain and mild chest and abdominal pain. P 95/min, Respirations 20/min, and BP 120/80. Exam shows severe tenderness of the cervical spine at C5. Bruise and mild tenderness over lower sternum and upper abdomen. Neuro exam is normal. CXR is normal except for slightly widened mediastinum. Cervical spine XR shows C5 facet fracture. Abdominal XR is normal. Most likely location of the life-threatening cardiovascular injury?
Thoracic aorta
NOT innominate artery
3) 19yo man brought to ER by police after found standing in his neighbor's living room in the middle of the night. He is conscious but remains mute during questioning. Temp 37C, respirations 18/min, BP 160/95. Exam shows bilateral nystagmus, constricted pupils, hypertonia, and decreased sensation to pinprick. Substance?
PCP
*Most people who use PCP become "spaced out" and appear mute, inactive, or even catatonic*
4) 4yo boy with fatigue since viral illness 3 weeks ago. Pale for 1 week, gums bled yesterday when brushing. Cervical, axillary, and inguinal adenopathy and hepatomegaly. Hb is 8, leukocytes 3000, platelets 30k. Most appropriate next step in management?
Bone marrow aspiration
*Not transfusion of pRBCs
*anyone presenting with aplastic crisis needs bone marrow biopsy to decide viral reaction versus cancer
*when expected answer not there, RETHINK AND PROCESS OF ELIMINATION--do not pick randomly!
*CARELESS* 5) 82yo F with visual loss in left eye since awakening. HTN treated with Lisinopril, and takes daily aspirin. Pupils are 2 mm bilaterally and reactive to light. Visual acuity is 20/30 on R and 20/400 on L. Fundoscopic exam of L eye shows dilated retinal veins and widespread retinal hemorrhages intermixed with patches of white exudate. R optic fundus wnl. Dx?
central retinal vein occlusion
NOT artery!
6) 160yo F brought in by her mom requesting birth control. Mom wants to talk to doc alone because daughter is staying out late, receiving many calls from several different boys, and wear tight clothing and excessive makeup. Daughter confides many details of the dates to her. Father is furious and berates daughter, so mother doesn't want to tell father about what is going on. On interview, she says she doesn't know why she is doing this, but would like to understand. Most appropriate next step in management?
Family therapy
*NOT psychodynamic psychotherapy for pt
*LOGIC; don't pick the highest sounding answer automatically
7) 6yo boy with cramping abdominal pain & right-sided scrotal pain for 4 hours. Vomited once, Exam shows distended abdomen. BS decreased, and diffuse tenderness to palpation with involuntary guarding. Right hemiscrotum discolored with swelling & tenderness superiorly. Left hemiscrotum is wnl. Most appropriate next step in management?
Operative procedure
NOT doppler
8) 37yo F with malaise, muscle aches, painful vulvar blisters, vaginal discharge, and dysuria for 3 days. Had sex with new partner 7 days ago. T 38. Exam shows bilateral painful inguinal lymphadenopathy and numerous 1-3 mm vesicles and ulcers on labia majora and minora, perineum, vulva, mons pubis. Next step in diagnosing these lesions?
Cx for herpes simplex
9) 24yo W with intermittent double vision and drooping of the eyelids for 3 weeks and difficulty chewing and swallowing for 1 week. Sx worse late in day. Eyelid ptosis worse on the right, weakness of abduction of right eye, adduction of left eye, and eye closure. Weakness of forehead and mouth. Speech is nasal. DTR and sensation are normal. Dx?
decreased acetylcholine receptors
NOT MS!
10) 75yo M with confusion and lethargy for 2 days. Was gardening on a 100F day before symptoms. 15-year Hx of DM treated with glyburide and 25-y Hx of HTN treated with HCTZ. Underwent lap chole 6 weeks ago. Smokes 1 pack daily and 2 drinks nightly. Traveled to Hawaii 2 months ago. T 41.5C, pulse 120/min, BP 90/60. Skin is hot and dry but not erythematous. Muscle tone decreased Serum CK is 8000, AST is 400. Cause?
Heat stroke
11) 72yo M with SOB for 3 days. Hx of HTN and CAD. Receiving 2 L/min of O2 via nasal canula. Temp 37C, P 110/min, resp 20/min, BP 150/80. Bilateral crackles and wheezes. HCT is 28%, leukocyte count is 8000. Pulmonary artery cath shows cardiac index of 2 L/min (N = 2.5 - 4.2) and a pulmonary artery occlusion pressure of 28. ABG shows pH 7.49; Pco2 30; Po2 58. Most appropriate next step in management?
Diuretic therapy
12) 32yo M with 3-month Hx of burning substernal chest pain and sour taste in his mouth. Sometimes awakens at night with acidic liquid in his mouth. Nonproductive cough for 2 months. Smoked 1 pack daily for 14 years. Drinks 6 beers every week. BMI 31. Exam is otherwise normal. Most appropriate next step in management?
Trial of omeprazole therapy
NOT Upper GI endoscopy!
13) 42yo F with intermittent loss of urine over past 3 weeks. Sx only after voiding. Pelvic exam shows 3-cm, midline, cystic, tender mass in the midthird of vagina. U/A is normal. Posvoid residual volume is 50 mL. Dx?
Urethral diverticulum
- The loss of urine only after voiding and cystic mass in the mid third of vagina suggest the diverticulum. During voiding, urine accumulates in the urethral outpouching ( diverticulum) and loss of urine occurs after voiding.
14) 12mo boy with persistent S. aureus abscess despite 2 weeks of cephalexin. 3rd infection since birth, including inguinal abscess with S. aureus, pneumonia and empyema. Cell type involved in Dx?
Neutrophil
(chronic granulomatous disease)
- susceptible to catalase positive orgs: Need PLACES (Nocardia, Pseudomonas, Listeria, Aspergillus, Candida, E coli, Staph aureus, Serratia)
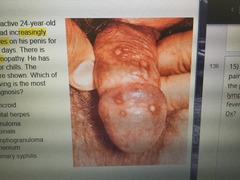
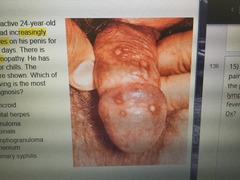
15) Sexually active 24yo M with painful sores on his penis for the past 5 days. There's lymphadenopathy. No fever/chills. Lesions are shown. Dx?
Genital herpes
- painful penil, vulvar or cervical vesicles and ulcers; can cause fever, HA, myalgia
OTHER
- chancroid (H ducreyi): painful genital ulcer with exudate, inguinal adenopathy
- lymphogranuloma venereum (C trachomatis L1-3): painless genital ulcers, painful lymphadenopathy (ie buboes), infection of lymphatics
- granuloma inguinale (Klebsiella granulomatis): ulcerative genital lesions in underdeveloped countries; Small, beefy-red bumps appear on the genitals or around the anus. The skin gradually wears away, and the bumps turn into raised, beefy-red, velvety nodules called granulation tissue. They are often painless, but they bleed easily if injured.
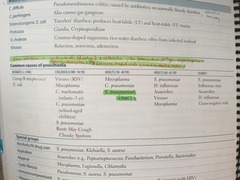
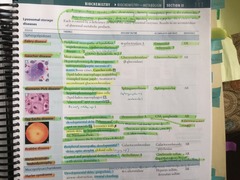
16) 43yo M with 3-day Hx of Temp 38.4C, left-sided chest pain, malaise, loss of appetite, and a cough productive of yellow phlegm and SOB. Smoked 2 packs/day for 25y. He appears ill. Pulse 112/min, resp 22/min, BP 118/72. Crackles and wheezes at left base, breath sounds decreased. Increased tactile fremitus and dullness to percussion at left base. CXR shown. Gram neg bacilli and leukocytes on stain. Dx?
H influenza
(CXR shows LLL opacity)
- Adults (18-40): Mycoplasma, c pneumo, s pneumo
- Adults (40-65): Strep pneumo, H flu
- Neonates (<4wk): GBS, Ecoli
17) 2 hours after repair of perforated gastric ulcer, 75yo W has multifocal PVCs. Hx of CHF treated with Digoxin and diuretics. Most likely abnormal serum concentration?
Decreased potassium
- Loop diuretics will cause hypokalamia and hypo magnesemia
- In acute toxicity, hyperkalemia is common
Chronic toxicity is often accompanied by hypokalemia and hypomagnesemia
18) 55yo F with metastatic breast cancer admitted for confusion progressing to obtundation over past 24 hours. Barely arousable. Most likely abnormal serum concentration?
Increased calcium (by way of PTHrP)
19) 32yo F at 16 weeks' gestation with 6-hours of fever and waxing/waning consciousness. Only meds is multivitamin with iron. T 38.3C. Neuro exam shows waxing/waning consciousness. HCT is 11%, platelets 52K, Cr is 3.5. Blood smear shows schistocytes. Dx?
Thrombotic thrombocytopenic purpura
- sx: pentad of neurologic and renal symptoms, fever, thrombocytopenia, and microangiopathic hemolygic anemia; also HUS in kids (ARF, microangiopathic hemolytic anemia, thrombocytopenia)
- Tx: plasmapheresis, steroids
20) 18yo F with fever, mild nonproductive cough, sore throat, general malaise, and anorexia for 5 weeks. Exudative pharyngitis with a whitish membrane, cervical LAD, and splenomegaly. Dx?
EBV
21) 27yo M with 2-month history of a rash on his face, neck, and torso. Rash began with couple tiny spots, and now there are more than 100. Exam shows 2-8 mm flesh-colored papules with central umbilication over face, neck, back, and chest. Dx with molluscum contagiousum is made. In addition to Rx, most appropriate intervention?
HIV antibody testing
NOT serologic testing for syphilis
22) 72yo M with decreased UOP 2 days after Rx for cholecystitis. UOP has been 15 mL/h for 3 hours. On admission, results showed gram neg bacteremia and DIC. CUrrently receiving IV fluids, cefoxitin, and gentamicin. Temp 38.5C, Pulse 110/min, resp 24/min, BP 90/64. Mild RUQ tenderness. Serum Cr increased from 1.5 2 days ago to 3. Urinalysis findings?
Blood 1+, Protein 1+, RBC 0-5, WBC 0-5, Casts pigmented granular, Other microscopic findings renal tubular epithelial cells
(ATN)
23) 77year old man is brought to the physician by family members because of progressive forgetfulness over the past 2 years. He rarely leaves the house and will no longer care for himself. His temperature is 36.2°C (97.2°F), pulse is 52/min, and blood pressure is 110/90 mm Hg. Abdominal examination shows no ascites. The liver is palpable 3 cm below the right costal margin. There is 2+ nonpitting edema of the lower extremities. Deep tendon reflexes are 1+, and sensation is intact. His gait is slow. He appears uninterested and responds to questions slowly. His Mini-Mental State Examination score is 20/30. Serum studies show -
Na+ 131 mEq/L
K+ 3.9 mEq/L
Creatinine 1.2 mg/dL
Alkaline phosphatase 160 U/L
AST 80 U/L
Hypothyroidism: decreased DTR, uninterested---assess for depression, bradicardia, hypoNaemia.
NOT vascular dementia because no focal neuro deficits
24) 70yo F with peeling, scaling, and cracking of the right nipple for 2 months. Breast exam shows no masses, and mammography shows no masses or calcifications. Dx?
Paget disease of the breast
NOT eczema
The symptoms of Paget's disease are similar to those of eczema of the nipple. However, if any of the following apply, an urgent referral to the breast cancer clinic should be performed:
-unilateral eczematous skin or nipple change that does not respond to topical treatment
-nipple distortion of recent onset
-spontaneous unilateral bloody nipple discharge
-male, aged 50 years and older with a unilateral, firm subareolar mass with or without nipple distortion or associated skin changes
25) 3 days after total hip replacement, 50yo M is unable to move his legs and has urinary incontinence. Sx began immediately following removal of epidural catheter inserted for pain control. His meds include ketorolac, enoxaparin, and morphine. Dx?
epidural hematoma
*taking enoxaparin
NOT residual neuro blockade from long acting anesthetic agents
26) 67yo M with aching in the calves while walking during the past 2 months, relieved by rest. Decreased pedal pulses. Symptoms due to narrowing of?
femoropopliteal arteries
27) Three days after hospitalization for treatment of severe muscle weakness secondary to Guillain-Barre
syndrome, a 21-year-old woman has a temperature of 39°C (102.2°F). Arterial blood gas analysis on 2 L/min of
oxygen via nasal cannula shows:
pH 7.33
P002 32 mm Hg
P02 50 mm Hg
An x-ray of the chest shows infiltrates in the middle and lower lobes. Bronchoscopy is performed; Gram stain of
material obtained from the right main-stem bronchus shows numerous segmented neutrophils, gram-positive
COCCI, and gram-negative cocci and bacilli. Which of the following is most likely to have prevented her acute
pulmonary symptoms?
Elevation of head of bed
(aspiration pneumonia)
NOT NG suction
28) 19yo African American man with 9-month Hx of watery diarrhea associated with abdominal cramps and bloating. Has occasionally had diarrhea after meals since age of 12, but has been worse since he started college 1 year ago. Exam shows no abnormalities. Cause of diarrhea?
Digestive enzyme deficiency
NOT "immunologic damage to the microvilli of the bowl,
-lactose intolerance. as oppose to say something like celiac's disease where if present since childhood he would have problems such as vitamins Deficiencies of some sort.
29) 37yo woman with progressive difficulty swallowing solids and liquids over the past 6 months. Had a 5Ib weight loss. Smoked 1.5 packs daily for 20 years. No alcohol. Abdominal exam nl. Upper endoscopy shows retained secretions in the esophagus and no mucosal lesions in the esophagus or stomach. Esophageal manometry most likely shows what?
Dec esophageal peristalsis, inc lower esophageal sphincter tone (achalasia)
The test typically reveals three abnormalities in people with achalasia:
-high pressure in the LES at rest
-failure of the LES to relax after swallowing
-an absence of useful (peristaltic) contractions in the lower esophagus
30) 16yo girl comatose next to a suicide note. Unresponsive. Temp 37.2C, p 100/min, resp 28/min, BP 100/66. Pupils reactive to light; doll's eye reflex present. Labs: Na 140, Cl 104, K 3.5, HCO3 6. ABG: pH 7.32, Pco2: 12; Po2: 92. What substance had she used in her suicide attempt?
Aspirin
(AG metabolic acidosis and respiratory alkalosis)
Winter's formula; PCO2 = 1.5 × [HCO3-]) + 8 ± 2
NOT methanol
31) Previously healthy 82 yo woman comes because she is concerned she has Parkinson Disease. Over 6 months, she has had occ difficulty finding word that she wants to use, her ability to distinguish smells has decreased. She reports that her reaction time to shifts in posture seems slow, and she needs to use a handrail to steady herself while walking on stairs. She loves alond, able to manage her own finances. Pupils 3 mm, mild reduction of upward gaze andbrisk rotatory nystagmus on left lateral gaze. Audio- high frequency hearing loss. No tremor or rigidity. Gait is normal. MMSE 29/30. Which of following warrants further evaluation?
Brisk rotatory nystagmus on left lateral gaze
NOT decreased upward gaze
32) 37 year old woman with sickle cell disease comes to physician because of a 24 hour history of fever, right upper abdominal pain after eating and nausea, last SC crisit was 5 months ago, only takes folic acid, 23BMI, T=100.8 pulse is 90 mild scleral icterus, abd distended, bowel sounds decreased, murphy sign present, ultrasonography shows cholelithiasis, pericholecystic fluid, normal commmonsized ZCBD,
Leuk=12,000
Bili=3
Alk phos=60
Amylase=90
Lipase=40
acute cholecystitis
33) 37yo F G3P3. Exam shows 3-cm, nontender, fluctuant mass involving left posterior vulva underlying the mucosa of the vestibule and external to the hymenal ring. Dx?
Bartholin duct cyst
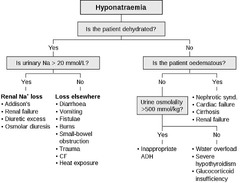
34) 72yo M for follow-up exam 4 weeks after 10-day quinolone Rx for UTI. Has been drinking 12 to 15 glasses of water daily to prevent another infection. 30-year hx of schizoaffective d/o. On Reisperidone. Oriented to person but not to place or time. P 80/min, BP 128/60, with no orthostatic changes. Exam shows dry oral mucosa and no JVD. Lungs clear. No peripherla edema. Muscle strength 5/5, sensation intact. Reflexes 1+ bilaterally. Labs: Na 122, K 4, Cl 94, HCO3 22, BUN 16, Cr 1.1; Urine: blood neg, glucose neg, protein neg, sodium 20, osmolality 200. Cause of hyponatremia?
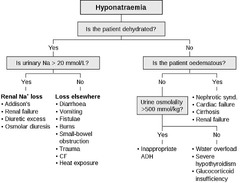
Psychogenic polydipsia
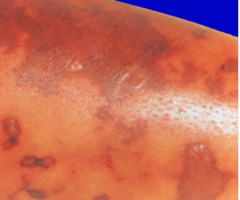
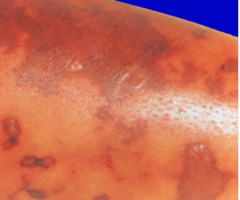
35) An 18 yo woman has had fever 12 hrs and obtundation 4 hrs. She had been attending a summer camp with 120 other students and was well until yesterday, when she developed a sore throat and nonproductive cough; this morning she couldn't be aroused. T= 101.5, P= 120, RR= 30, BP= 80/50. Extremities cool. Skin lesion shown over her extremities, chest and abdomen. Hsct 41%, leuko 21200 with shift to left. Dx?
Meningococcemia (Neisseria meningitis)
There may be few symptoms at first. Some may include:
Fever
Headache
Irritability
Muscle pain
Nausea
Rash with red or purple spots
Later symptoms may include:
A decline in your level of consciousness
Large areas of bleeding under the skin
Shock
36) Five days after undergoing an open splenectomy for immune thrombocytopenic purpura, a 57 year old woman has the onset of shortness of breath. During the operation, dissection of the splenic hilum was difficult. Her only medication is morphine. Her temperature is 37.3°C (99.2°F), pulse is 80/min, respirations are 20/min, and blood pressure is 120/80 mm Hg. The surgical wound appears normal. Breath sounds are decreased at the left lung base. Her leukocyte count is 15,600/mm , platelet count is 112,000/mm , and serum amylase activity is 90 U/L. Which of the following is the most appropriate next step in management?
CXR (unsure)
37) Newborn with B/L clubfoot deformity. Born at term following uncomplicated preg and delivery. Did not more his lower extremities immediately after birth, did not cry when he receied a needlestick in his feet. On exam, he is vigorous and moves his upper extremirites but not his lower extremities. Bladder is palpable and full, Dx?
Spinal dysraphism
NOT cerebral palsy
In spinal dysraphism:
Look for h/o tufts of hair , (which is not present in this case) but if u see the child can move upper extremities and not lower ext, also no sensation in lower ext ( note: this does not happen in CP---In CP there will be weakness involving both upper/lower ext in the form of spacticity or wherever the hypoxic injury has injured the part of the brain,but not such discrepancy (only lower ext affected with upper ext being normal in above vignette )since the brain is involved in CP ---brain injury due to hypoxia/vascular insufficiency mostly inutero)
vs spinal dysraphism--- is an umbrella term and neural tube defects come under it ;the tufts of hair with tethered cord is one of the occult spinal dysraphism ,
Here spinal cord /peripheral nerves is affected and the above vignette has clearly mentioned lower ext weakness and no sensation in lower ext but the child is moving upper ext (spared); also bladder is full so lesion is below the spinal cord involved ,most likely tethered cord in this case!!
also, club foot (another hint) associated with spinal dysraphism!!
38) 77 year old man brought to the emergency deparment after 15 minutes since the onset of cough productive of large amounts of blood tinged sputum, life long history of chronic productive cough and recurrent episodes of pneumonia in the right lower lobe of the lunge, 15 minutes after arriving the bleeding stops spontaneously his temp is ok, pulse is 110, resp 24, bp OK exam shows bronchophony in the right lateral lungm CXR shows thin walled cystic spaces in the right lower loe with some air fluid levels., which is the most likely explanation of these findings?
Destruction and dilation of distal airways
.Bronchiectasis...Lung CXR might be showing Lung abscess...
Lung abscesses can be classified based on the duration and the likely etiology. Acute abscesses are less than 4-6 weeks old, whereas chronic abscesses are of longer duration. Primary abscesses are infectious in origin, caused by aspiration or pneumonia in the healthy host. Secondary abscesses are caused by a preexisting condition (eg, obstruction), spread from an extrapulmonary site, bronchiectasis, and/or an immunocompromised state.
39) 4 yo boy develops chickenpox 8 hrs after visiting his NB sister in nursery. Six other full term NB were also exposed, all of the mothers have a H/O chickenpox prior to pregnancy. Which of the following is most appropriate recommendation to prevent chickenpox in NB?
No intervention is necessary.
NOT administration of varicella vaccine to newborns with negative varicella titers
40) A previously healthy 10 y/o girl is brough to the physician because of a 2 day history of mildly itchy rash that has spread from her face to her chest, arms, and legs. One week ago, she had a 2-day history of low grade fever, HA, and malaise. She has not had a sore throat. She appears well. Her temp is 37.3 (99.1). A photograph (showing red cheeks) is shown. The rash over the chest and upper and lower extremities is symmetric, maculopapular, reticular, erythematous and nonconfluent. The remainder of the exam shows no abnormalities. Which of the following is the most appropriate next step in pharmacotherapy?
None indicated (parvovirus)
41) An 87-year-old man comes to the physician because of a 1-year history of difficulty starting his urinary stream and occasional postvoid dribbling. He typically arises to void two times nightly. He has a 30-year history of type 2 diabetes mellitus complicated by orthostatic hypotension secondary to autonomic dysfunction.Current medications include lisinopril and glyburide. His blood pressure is 140/80 mm Hg while supine and 100/60 mm Hg while standing. Examination shows an enlarged prostrate. Which of the following is the most appropriate pharmacotherapy for this patient's urinary symptoms?
Finasteride (5alpha reductase inhibitor)
NOT doxazosin (alpha blocker) due to orthostatic hypotension
42) 32 yo W brought to ER, 2 day hx of vomiting, diarrhea and right sided pelvic pain. Last mentrual period was 3 wks ago. Temp 102.2, RR20, P100, BP 120/70. Abdo exam shows right lower quadrant tenderness with rebound. Decreased bowel sounds. Pelvic exam shows right adnexal tenderness. Negative serum pregnancy test. Labs: Hg 12 Leukocytes 15,000 Seg PMNs 80% Bands10% Lymphs5% Monos 5%. Ultrasound shows no adnexal masses. Most likely dx?
Appendicitis
NOT adnexal torsion (can't have torsion if no mass)
43) A previously healthy 21 years old woman comes to the physician 1 day after the sudden onset of severe right sided chest pain that increases with deep inspiration. During this period she has had shortness of breath and difficulty taking a deep breath. She has had no cough. Yesterday she returned from a 3 weeks vacation to the Andes mountains. She does not smoke cigarettes, drink alcohol or use illicit drug. Her temperature is 38 C (100.4 F), pulse is 80/min, respiration is 14/min and blood pressure is 100/80 mmHg. Examination shows a faint macular,non pruritic,erythematous rash over the cheeks and trunk. There is dullness to percussion at the right lung base and an inspiration rub with no crackles and wheezes. Which is the most likely diagnosis?
viral pleurisy
INSPIRATION RUB with no crackles and the very first line saying CHEST PAIN INCREASING IN "DEEP INSPIRATION"==== PLEURAL RUB
44) 57yo M with generalized weakness and purple rash on his legs for 3 days. He has a hx of several blood transfusions. Exam shows 1.5-cm, raised, nonblanching purple lesions over the legs. Positive cyroglobulins diagnosed with essential mixed cryoglobulinemia. Negative hepatitis C. Rx?
Interferon-alpha
45) 82 year old man with CHF comes to doc for f/u exam. one month ago, he had worsening dyspnea while lying in bed at night and walking up stairs, and his dose of furosemide was increased. his only other medication is lisinopril. he was dx with chef 5 years ago after MI. he had coronary angiography and stent at that time. no CP since them. also has a 10 year hx of well controlled CKD. creatinine conc have ranged from 1.3- 1.5 and urinalyses have shown no protein. today his pulse is 90/min, rest are 14/min and BP is 130/86/ cardiopulmonary shows no abnormalities. there is trace edema of ankles, which has decreased since examination 1 month ago. serum studies show:
1 month ago: na-138, K 4, cl 101, HCo3- 26, bun-15, cr-1.8
today: NA-140, k-4.2, cl-103, hco3-28, bun-24, cr-2.3
urinalysis shows no abnormalities. which of the following is the most likely explanation for the change in lab values during the past month?
Decreased renal blood flow
Increasing the dose of furosemide increases fluid lost as evidenced by his decreased pedal edema. A decrease in body fluid = decreased in blood reaching the glomerulus = kidney not able to maintain GFR = rise in c
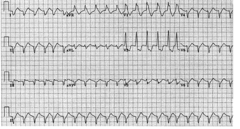
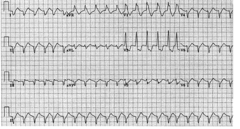
46) 70 yo W brought to ER 3hrs after onset of substernal chest pain, weakness and dsypnea. She had MI 6 months ago and has had recurrent chest paon on exertion treated with nitroglycerin. T98.8, rr 22, bp 60/40. Exam is normal. EKG is shown. Dx?
Ventricular tachycardia
47) A 67 yo man has had an ulcer on ant surface of leg just above ankle for 2 wks. He had MV replacement 15 yrs ago because of Rheumatic valvular disease. Takes furosemide for CHF and oral hypoglycemic for DM II. Exam- 5 cm ulcer with 3 mm red border. There is moderate edema from toes to midcalf bilaterally; his feet are warm, pulses weakly palpable. Scattered crackles are heard at lung bases B/L. Dx?
Stasis dermatitis with ulcer
(moderate edema)
NOT arterial insufficiency
48) 62yo M with 12hr history of fever and generalized muscle pain. He has leukemia treated intermittently with cehmo through a catheter. Exam shows a yellow discharge at the catheter insertion site. Gram stain of the discharge shows GP cocci in clusters. Cultures are ordered. In addition to removing the catheter, which abx?
Vancomycin
- Use: GP bugs only--serious multidrug resistant orgs including MRSA, S epidermidis, Enterococcus, C diff
- SE: NOT trouble free=Nephrotoxicity, Ototoxicity, Thrombophlebitis
NOT clindamycin: anaerobic infections (Bacteroides, Clostridium perfringens) in aspriation pneumonia, lung abscesses and oral infections
49) 10 yo girl fever and joint pain 5 days. T= 103, P = 120, RR= 24, BP= 110/70. Precordial heave. Gallop and grade 3/6 holosystolic murmur in 4th IC space at midclavucular line. Elbow and knee tender. GAS, ASO increased. Explanation for the cardiac findings?
Mitral valve incompetence
(holosystolic NOT diastolic)
NOT MV stenosis
#urine specific gravity results will fall between ___
1.002 and 1.030 if your kidneys are functioning at a normal level
#normal JVD range
The normal distance is <4cm above sternal angle; add 5cm to this because the right atrium is 5cm below the sternal angle.
#Pt with asthma and CF presents with 3 month history of progressive cough that has become thick yellow occasionally tinged with blood. serum IgE 1250. CXR shwos linear atelectasis at the lung bases and thickened airways and irregular cystic opacities primarily in a central distribution
allergic bronchopulmonary aspergillosis (fungal)
- may cause bronchiectasis and eosinophilia
#Pt with multiple myeloma most susceptible to infection with...?
Streptococcus pneumoniae
#37 yo M persistent numbness in hands/feet for 10 months, weakness in L wrist for 3 weeks. He renovates old houses. he has abdominal pain and diagnosed with gastritis. BP is 135/95. mucous mb pale. Neuro exam shows weakness with dorsiflexion of L wrist and loss of sensation in stocking glove distribution. He has low hematocrit and BUN is 35. Blood smear shows microcytic hypochromic erythrocytes. Early tx with what would have prevented him?
sodium calcium edetate (edetate calcium disodium) and succimer (DMSA) in the treatment of inorganic lead poisoning
In children, symptoms can include:
Slightly lower intelligence and smaller size compared to children of the same age.
Behavior problems, such as acting angry, moody, or hyperactive.
Learning problems.
Lack of energy, and not feeling hungry.
In adults, lead poisoning can cause:
Changes in behavior, mood, personality, and sleep patterns.
Memory loss and trouble thinking clearly.
Weakness and muscle problems.
Headaches.
#Previously healthy 18 yr old woman, lump in her neck she first noticed 1 month ago. Otherwise asymptomatic. Exam shows 3cam left supraclavicular lymph node that is firm and rubber. Spleen is 3cm below left costal margin. Remaining exam is normal. Labs will most likely show which?
non hodgkins lymphoma has increased LDH
What does elevated GGT (gamma glutamyltransferase) entail?
Alcoholic cirrhosis or individuals who are heavy drinkers
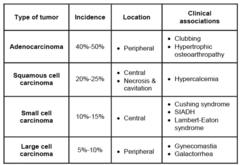
Pt with 7cm right lower lobe mass with some scatter calcifications. The lesio abuts the posterior chest wall without clear invasion. Right lymph nodes positive. 1.5cm mass in right adrenal gland.
Non small cell lung carcinoma
NOT mesothelioma (malignancy of the pleura associated with asbestosis)
Fever, neutropenia and intracellular inclusion bodies in the transplanted organ
CMV syndrome (ganciclovir)
9yo M with progressive proximal muscle weakness and a purple red discoloration over his cheeks and upper eyelids over the past 8 weeks. Symptoms began shortly after a camping trip. No tick bite exposure. PE=purple red discoloration over the cheeks and eyelids; periorbital edema, erythematous plaques and scales over the elbows and knees, and flat topped red papules over all knuckles. Generalized weakness and atrophy of the proximal muscles.
Dermatomyositis
37yo Type I DM admitted or inadequate control of his glucose conc for the past 2 months. Non compliant with meds. Wants to leave hospital. Fasting glucose is 120 mg/dL. Next step?
Adhere to pt's wishes and discuss home cares ptions
Pregnant woman with urine dipstick showing leukocyte ester are; UA shows WBcs and rare GN rods. Next step?
Oral amoxicillin therapy
!How to manage second trimester pregnancy with elevated maternal serum alpha fetoprotein?
US (not triple screen or repeat or amniocentesis)
Opening snap followed by a low pitched diastolic murmur at that their left intercostal space; CXR shows LA enlargement
MV stenosis
2mo M with 6 week history of persistent diarrhea and vomiting, most pronounced after formula feeding. Some weight loss since birth. Irritable, jaundice, hepatosplenomegaly. Hypoglycemia, 3+ reducing substances in urine
Classic galactosemia (decreased gluconeogenesis)
- absence of galactose 1 phosphate uridyltransferase ; accumulation of toxic substances
- autosomal recessive
- Sx: failure to thrive, jaundice, hepatomegaly, infantile cataracts, intellectual disability, +reducing substances in urine
- Tx: exclude galactose and lactose (galactose+glucose) from diet
****
4. classic galactosemia.. as they have decreeased ATP and accumulation of Gal-1-P... less glu-1 phosphate for gluconeogenesis... and also a lot of aldose reductase activity .. which leads to reducing stuff in urine.. also note in the question .... after feeds sumtime the symptoms develop... as lactose broken down to gluc and galact.. galact is not metabolised .. so leads to hypoglycemia... very important condition ... treat by avoiding strictly breast feed or milk .. but soy milk bsed diet is good.... so Decreased gluconeogenesis is the answer.
GSW to abdomen. P120, RR28, BP70/40. Breath sounds decreased on left. Entrance wound in LUQ at midclavicular line below the left costal margin and exit wound in the left axillary line at the 4th rib. IV fluids started. Next step?
Left tube thoracostomy
(NOT intubation or CXR or peritoneal lavage)
62yo white man with 8 month history of progressive pain and stiffness of his hands; dark brown skin; heart failure; heberden nodes; negative RF. Dx and Tx
Dx: hemochromatosis
Tx: phlebotomy
17yoF with 2 month history of exercise induced cough and nasal congestion. Normal PFTs.
Asthma
(Variable intrathoracic upper airway obstruction = tumor in lower trachea)
2d after hospital admission for CHF, pt unable to walk due to severe throbbing pain in his left out. Fever. Tenderness, erythema and edema of the left great toe; active and passive ROM produces pain.
Gout (20,000 WBC, needle shaped, no org)
17yo F with 1 week history of itching and progressive rash. Her sister whom she shares a room with had similar symptoms. PE=multiple 2-5mm erythematous papules over the trunk, esp at the waistline, and over the forearms, hands and fingers. Cause?
Sarcoptes scabei
(NOT VZV!)
Four days after bone surgery after MVA, pt still experiences agitation and confusion despite treatment with haloperidol. Exam shows tremulousness. Oriented to person only.
Alcohol withdrawal
(Not adverse effect to medication)
Jackhammer operator with pain and swelling of right arm for 3D. Sx moderately exacerbated by exertion. PE=right upper extremity shows erythema and moderate edema.
Axillary subclavian venous thrombosis
NOT thoracic outlet syndrome: compression of vessels in space between the collarbone and first rib; pain in the shoulder and neck and numbness, weakness and coldness of fingers
How to treat bilateral paravertebral muscle spasm
Regular activity
(NOT bed rest!)
Male pt with 3 nontender, sessile, flesh colored lesions on the shaft of the penis that are 10mm in diameter. On application of a dilute solution o acetic acid, lesions turn white.
Genital warts (HPV)
- Tx: cryotherapy
Pt with stab wound to chest. Low BP, yes JVD. PE=2cm at the left 6th intercostal space at the midclavicular line. Heart sounds not audible. Next step
Pericardiocentesis (NOT echo)
Pt with serum cholesterol of 290mg/dL (TG 300). Drinks a pint of vodka daily. Next step
Alcohol cessation
Pt has worsening pain and swelling of her right knee for the past 2 days. She must stand often while working. Right knee is erythematous, swollen and tender; there is pain on movement. X ray of the knee shows an effusion but no structural abnormalities
Arthrocentesis of the knee
(READ carefully)